Gastroesophageal Reflux Disease
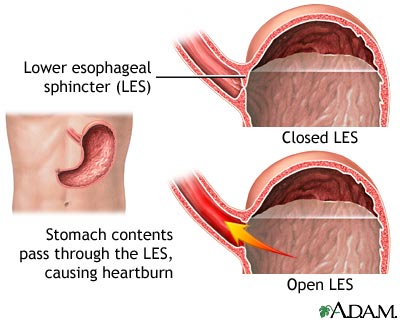
Gastroesophageal reflux disease, or GERD, occurs when the lower esophageal sphincter (LES) does not close properly and stomach contents leak back, or reflux, into the esophagus. The LES is a ring of muscle at the bottom of the esophagus that acts like a valve between the esophagus and stomach. The esophagus carries food from the mouth to the stomach
When refluxed stomach acid touches the lining of the esophagus, it causes a burning sensation in the chest or throat called heartburn.The fluid may even be tasted in the back of the mouth, and this is called acid indigestion.
Occasional heartburn is common but does not necessarily mean one has GERD. Heartburn that occurs more than twice a week may be considered GERD, and it can eventually lead to more serious health problems.
Anyone, including infants, children, and pregnant women, can have GERD.
What are the symptoms of GERD?
The main symptoms are persistent heartburn and acid regurgitation. Some people have GERD without heartburn. Instead, they experience pain in the chest, sore throat, hoarseness in the morning, or trouble swallowing. You may feel like you have food stuck in your throat or like you are choking or your throat is tight. GERD can also cause a dry cough and bad breath.
What causes GERD?
No one knows why people get GERD. A hiatal hernia may contribute. A hiatal hernia occurs when the upper part of the stomach is above the diaphragm, the muscle wall that separates the stomach from the chest. The diaphragm helps the LES keep acid from coming up into the esophagus. When a hiatal hernia is present, it is easier for the acid to come up. In this way, a hiatal hernia can predispose to reflux.
Other factors that may contribute to GERD include:
- alcohol use
- excess weight
- pregnancy
- smoking
Also, certain foods can be associated with reflux events, including:
- citrus fruits
- chocolate
- drinks with caffeine
- fatty and fried foods
- garlic and onions
- mint flavorings
- spicy foods
- tomato-based foods, like spaghetti sauce, chili, and pizza
Modifying your diet to reduce or eliminate these items can greatly reduce GERD symptoms.
How is GERD treated?
If you have had heartburn or any of the other symptoms for a while, you should see your doctor. You may want to visit an internist (a doctor who specializes in internal medicine) or a gastroenterologist (a doctor who treats diseases of the stomach and intestines). Depending on how severe your GERD is, treatment may involve one or more of the following lifestyle changes and medications or surgery.
Lifestyle Changes
- If you smoke, stop.
- Do not drink alcohol.
- Lose weight if needed.
- Eat small meals.
- Change your diet to eliminate those foods and beverages which aggravate GERD.
- Wear loose-fitting clothes.
- Avoid lying down for 3 hours after a meal.
- Raise the head of your bed 6 to 8 inches by putting blocks of wood under the bedposts Ð just using extra pillows will not help.
Medications
Your doctor may recommend over-the-counter antacids, which you can buy without a prescription, or medications that stop acid production, or others which help the muscles that empty your stomach.
Antacids, such as Maalox, Mylanta, Pepto-Bismol, Rolaids, and Riopan, are usually the first drugs recommended to relieve heartburn and other mild GERD symptoms. Many brands on the market use different combinations of three basic salts magnesium, calcium, and aluminum – with hydroxide or bicarbonate ions to neutralize the acid in your stomach. Antacids, however, have side effects. Magnesium salt can lead to diarrhea, and aluminum salts can cause constipation. Aluminum and magnesium salts are often combined in a single product to balance these effects.
Calcium carbonate antacids, such as Tums, Titralac, and Alka-2, can also be a supplemental source of calcium. They can cause constipation as well.
Foaming agents, such as Gaviscon, work by covering your stomach contents with foam to prevent reflux. These drugs may help those who have no damage to the esophagus. They can also minimize excess belching.
H2 blockers, such as cimetidine (Tagamet HB), famotidine (Pepcid AC), nizatidine (Axid AR), and ranitidine (Zantac 75), impede acid production. They are available in prescription strength and over the counter. These drugs provide short-term relief, but over-the-counter H2 blockers should not be used for more than a few weeks at a time without physician supervision. They are effective for about half of those who have GERD symptoms. We strongly recommend that you consult with a physician before using these on a long-term basis.
- Proton pump inhibitors include omeprazole (Prilosec), lansoprazole (Prevacid), pantoprazole (Protonix), rabeprazole (Aciphex), and esomeprazole (Nexium), which are all available by prescription and many are generic. Prilosec OTC and Prevacid is now available over-the-counter. Proton pump inhibitors are more effective than H2 blockers and can relieve symptoms in almost everyone who has GERD. Both these medications are taken 30-60 minutes before eating. Again, since persistent heartburn symptoms can indicate a number of more serious conditions, we strongly recommend discussing this medication with your physician before choosing to take it for an extended period of time.
Another group of drugs, prokinetics, helps strengthen the sphincter and makes the stomach empty faster. This group includes bethanechol (Urecholine) and metoclopramide (Reglan). Metoclopramide also improves muscle action in the digestive tract, but these drugs have frequent side effects that limit their usefulness.
Because drugs work in different ways, combinations of drugs may help control symptoms. Your doctor is the best source of information on how to use medications for GERD.
What if GERD symptoms persist?
If your heartburn does not improve with lifestyle changes or drugs, you may need additional tests.
- A barium swallow radiograph uses x-rays to help spot abnormalities such as a hiatal hernia and severe inflammation of the esophagus. With this test, you drink a solution and then x-rays are taken. Mild irritation will not appear on this test, although narrowing of the esophagus called stricture – ulcers, hiatal hernia, and other problems will. This test is rarely used these days.
- Upper endoscopy is more accurate than a barium swallow radiograph and may be performed in a hospital or a doctor’s office. The doctor will spray your throat to numb it and slide down a thin, flexible plastic tube called an endoscope. A tiny camera in the endoscope allows the doctor to see the surface of the esophagus and to search for abnormalities. If you have had moderate to severe symptoms and this procedure reveals injury to the esophagus, usually no other tests are needed to confirm GERD.
The doctor may use tiny tweezers (forceps) in the endoscope to remove a small piece of tissue for biopsy. A biopsy viewed under a microscope can reveal damage caused by acid reflux and rule out other problems if no infecting organisms or abnormal growths are found. - In an ambulatory pH monitoring examination, the doctor puts a tiny tube into the esophagus that will stay there for 24 hours. While you go about your normal activities, it measures when and how much acid comes up into your esophagus. This test is useful in people with GERD symptoms but no esophageal damage. The procedure is also helpful in detecting whether respiratory symptoms, including wheezing and coughing, are triggered by reflux. A wireless version of this test is also available to detect acid reflux over a 48 hour period (Bravo testing).
Surgery for GERD
Surgery is an option when medicine and lifestyle changes do not work. Surgery may also be a reasonable alternative to a lifetime of drugs and discomfort.
Fundoplication, usually a specific variation called Nissen fundoplication, is the standard surgical treatment for GERD. The upper part of the stomach is wrapped around the LES to strengthen the sphincter and prevent acid reflux and to repair a hiatal hernia.
This fundoplication procedure may be done using a laparoscope and requires only tiny incisions in the abdomen. To perform the fundoplication, surgeons use small instruments that hold a tiny camera. Laparoscopic fundoplication has been used safely and effectively in people of all ages, even babies. When performed by experienced surgeons, the procedure is reported to be as good as standard fundoplication. Furthermore, people can leave the hospital in 1 to 3 days and return to work in 2 to 3 weeks.
Endoscopic devices, The U.S. Food and Drug Administration (FDA) has approved several endoscopic devices to treat chronic heartburn. The Bard EndoCinch system puts stitches in the LES to create little pleats that help strengthen the muscle. The Stretta system uses electrodes to create tiny cuts on the LES. When the cuts heal, the scar tissue helps toughen the muscle. The long-term effects of these two procedures are unknown. Endoscopic devices are rarely used in the management of GERD.
What are the long-term complications of GERD?
Sometimes GERD can cause serious complications. Inflammation of the esophagus from stomach acid causes bleeding or ulcers. In addition, scars from tissue damage can narrow the esophagus and make swallowing difficult. Some people develop Barrett’s esophagus, where cells in the esophageal lining take on an abnormal shape and color, and which over time can lead to cancer.
Also, studies have shown that asthma, chronic cough, and pulmonary fibrosis may be aggravated or even caused by GERD.
Points to Remember
- Heartburn / acid indigestion, is the most common symptom of GERD. Anyone experiencing heartburn twice a week or more may have GERD.
- You can have GERD without having heartburn. Your symptoms could be excessive clearing of the throat, problems swallowing, the feeling that food is stuck in your throat, burning in the mouth, or pain in the chest.
- If you have been using antacids for more than 2 weeks, it is time to see a doctor. Most doctors can treat GERD. Or you may want to visit an internist–a doctor who specializes in internal medicine–or a gastroenterologist–a doctor who treats diseases of the stomach and intestines.
- Doctors usually recommend lifestyle and dietary changes to relieve heartburn. Many people with GERD also need medication. Surgery may be an option.
For More Information
American College of Gastroenterology (ACG)
American Gastroenterological Association (AGA)




